FDA 510(k) Process Explained: What to Know About Premarket Notification

FDA 510(k) Process Explained: What to Know About Premarket Notification
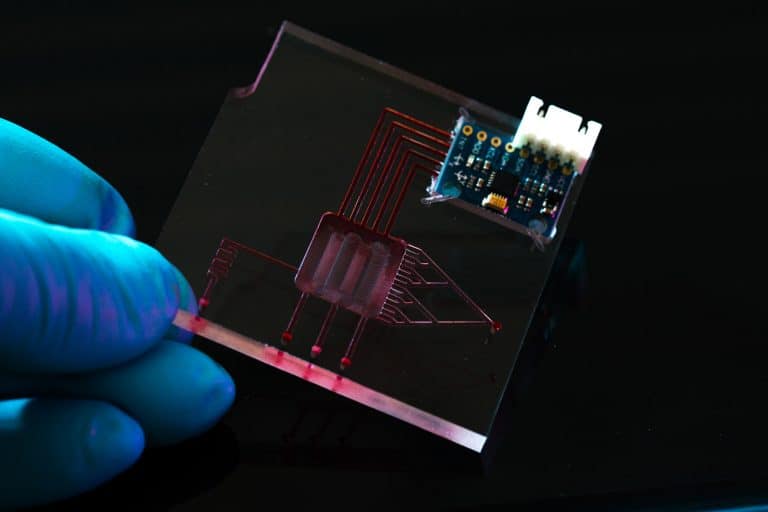
For companies looking to bring moderate-risk medical devices to market, navigating the FDA’s 510(k) premarket notification process is essential and often complex. This guide breaks down the fundamentals of a 510(k): what it is, how the process works, and the practices that can make or break your submission, but most importantly, it emphasizes the need to focus not only on securing clearance, but also on achieving market success by ensuring your device is intuitive, needed, and ready to perform — a methodology at the heart of Cortex Design.
What Is a 510(k)?
510(k) is a type of premarket submission you file with the FDA to demonstrate that your medical device is substantially equivalent to a legally marketed device, known as a predicate. By proving substantial equivalence to an existing product, you can avoid the costs and delays of recertification or new clinical trials.
When Is a 510(k) Required?
Not every medical device requires the 510(k) process. There are several types of market submissions. Generally, 510(k) submissions are intended for Class II devices, which the FDA considers medium-risk. They’re not life-sustaining like many Class III devices, but they are significantly more complex than Class I products. Class II devices typically require more rigorous evidence of safety and effectiveness than Class I, but you can meet these requirements by demonstrating substantial equivalence instead of conducting new clinical trials. See more on device classification here.
| Class | Examples | Regulatory pathway |
|---|---|---|
| Class I | Non-powered (e.g., dental mirrors, manual stethoscopes), bandages, examination gloves | General controls: list device, register establishment, follow GMP/QSR, maintain DMR and DHF. Usually 510(k)-exempt, unless “reserved”. Note: If novel, may require De Novo submission. |
| Class II | Moderate-risk tools used outside hospitals/clinics, closer to the home/patient (e.g., powered wheelchair, pregnancy tests) | 510(k) submission. Notes: Some Class 2 devices are 510(k)-exempt. If no predicate exists, may require De Novo submission. |
| Class III | Life-sustaining or high-risk implants (e.g., pacemakers, heart valves) | Premarket Approval (PMA) |
510(k) Core Requirement: Demonstrating Substantial Equivalence
The core of a 510(k) submission is showing that the new device is substantially equivalent to an existing product in terms of intended use, technological characteristics, and risk profile – this is the predicate. Your submission needs to demonstrate that your medical device doesn’t raise new safety or effectiveness concerns.
Finding a predicate through the FDA 510(k) database and other tools
The FDA maintains a database that allows you to search for cleared devices that can serve as benchmarks for substantial equivalence. In it, you can review their manufacturer, classification, clearance date, who they claim equivalence to, and more. There are also specialized open-source or commercial AI tools that can accelerate the discovery of suitable predicates.
But be cautious! There are many challenges in predicate discovery.
- Poorly documented – What seems like a perfect predicate may mislead your development process by misrepresenting its actual technology or performance. You must carefully assess technological characteristics and risk profiles, and may need to reverse-engineer the requirements for that particular device or find substantial equivalency elsewhere.
- Older devices – They may have been cleared under older standards and may not meet current regulatory requirements, such as updated sterilization or cleanability guidelines.
- Bad performance – Just because the device is on the market doesn’t mean it’s doing well. It may have recalls or user complaints. These are documented, so it’s wise to check the MAUDE database for any safety concerns, recalls, or complaints related to potential predicates.
“Finding a predicate is only the first step. Finding the substantial equivalency to the predicate and demonstrating that, that’s the real challenge. That means going beyond what you see in databases or AI tools.”

How close does your predicate device need to be?
The FDA primarily cares about risk and safety. Your device’s form factor can be different as long as it delivers therapy or diagnostics in the same way as the predicate. On the other hand, if your treatment method is significantly different, this will introduce new risks and may not qualify as substantially equivalent.
An efficient way to assess your predicate is through the FDA’s Q-Submission (Q-Sub) Program, specifically the Pre-Submission (Pre-Sub) process. This allows you to ask specific questions, such as “Is the proposed predicate device appropriate if we can demonstrate substantial equivalence?” and receive formal feedback from the FDA.
The 510(k) Process and Timeline
There is no single “correct” method to prepare and execute a 510(k) submission. The strategy depends on several factors, including the stage of product development, available financing, and the internal or external expertise a company can leverage.
Common but flawed approach: Starting at the end (back-documenting)
Many organizations attempt to “start at the end.” In this scenario, they engage a regulatory specialist only after the device is largely developed and seemingly ready for market. Only then would they initiate the integration of a quality management system (QMS) and generate the documentation required for the 510(k) submission. They are essentially “back-documenting” — retroactively creating records to satisfy regulatory requirements based on activities already completed. This approach is generally considered poor practice and is cautioned against at Cortex Design. It increases the risk of documentation gaps and inconsistencies that can delay or jeopardize clearance.
Recommended approach: Starting with the end in mind
A more effective strategy involves planning with the end goal in mind right from the start. This means:
- Engaging a regulatory specialist early in the development process, ideally one with specific experience in the relevant device category. (You can do this yourself, or have Cortex help you with this.)
- Collaboratively integrating that specialist into your development process, so they can help you build the right quality management framework and documentation from day one.
- Embedding regulatory and quality considerations into the product lifecycle proactively, rather than attempting to reconstruct them after design completion.
Recommended process and timeline of a 510(k) submission
The process should begin when you have a functioning prototype — something that looks technically promising, the device is substantially derisked, and there’s clear evidence of market demand. From there, on a high level, the process would follow this timeline:
- Define the user and intended use: This creates the foundation for your design controls — the documented requirements your device must meet.
- Document evolving design controls: As development progresses, your design controls will likely evolve. It’s crucial to document all these changes in your Design History File (DHF), including formative usability studies and how users were involved in shaping decisions.
- Finalize for submission: All the above culminate in your Device Master Record (DMR) (and DHF), the definitive blueprints for consistent production. With all documentation and validation complete, it’s time to prepare your submission using the FDA’s eSTAR PDF template for structure and guidance, and file it electronically through the appropriate FDA portal.
The goal of this process is to demonstrate that your device is safe and effective. But it’s important to note that safety and effectiveness alone don’t guarantee commercial success.
That’s why at Cortex, we encourage teams not to just focus on checking regulatory boxes, but to think holistically about how their device will fit into the broader healthcare and business landscape. For example, will it be reimbursed? Will it be better than what’s already out on the market?
How long does the 510(k) process take?
From a benchtop prototype to a complete market submission, it’s rare for this process to take less than a year. In reality, most medical device startups operate for five to nine years before reaching market, due to the capital and iterative development required.
Cortex Design’s Unique Approach to the 510(k)
We don’t treat the 510(k) process as a checklist to complete after the fact. Its elements are integrated into the way we design from the start—but that’s because our priority is to design the right product: one that’s safe, effective, user-centered, and commercially viable. From that foundation, we conceptualize the right medical device through our design process and document requirements—grounded in real design intent—during the engineering phase.
“We’re not just checking boxes, like ‘we made this choice for a button, or we made this choice for a display.’ It needs to be part of the process of design to make those choices in the first place. That’s really our differentiator.”
How Involved Should a Client Be?
This ultimately depends on the client; their experience, their desired level of involvement, and at what stage, etc. But at Cortex Design, we work best with highly engaged clients, simply because 510(k) submissions are truly a collaborative effort.
While we typically take the lead on design, documentation, DHF, and the verification work needed to show that design inputs have been met, other elements – such as final validation studies or detailed regulatory strategy – may be led by the client, a third party, or by us, depending on what best fits the project. Regardless of how responsibilities are split, we ensure our clients stay closely involved in the decisions that shape both clinical and market success. It’s always a collaborative effort, working together toward a commercially successful product.
Common Mistakes that Delay an FDA 510(k) Clearance
Several mistakes frequently lead to delays or even rejections during the 510(k) review process:
- Selecting a predicate that isn’t substantially equivalent: Devices that are too old (cleared under old standards), poorly documented or currently underperforming will mislead your development and ultimately cost you time and money.
- Failing to apply current standards: Beyond the predicate, your device must also independently meet all applicable, up-to-date regulatory standards. Just matching an existing device isn’t enough if new testing protocols or safety requirements apply.
- Submitting incomplete or unclear documentation: Poorly prepared submissions increase the likelihood of FDA reviewers requesting additional information, delaying the clearance process and increasing costs.
Note: FDA reviewers are under more pressure than ever, especially given recent budget constraints and staffing shifts. That means the quality of your submission package is critical.
The best strategy is to do thorough research and prepare a comprehensive, well-organized submission that minimizes ambiguity, reduces costly back-and-forth with the FDA, and improves your chances of first-round clearance.
At Cortex, it’s our responsibility to make sure that all the pieces of the 510(k) submission are carefully reviewed so nothing critical is missing or poorly prepared. This thorough review work can be led entirely by Cortex, or it can be done together with a regulatory specialist that the client already has on their team.
Best Practices for 510(k) Submissions
Staring at the right time
Effective 510(k) planning should begin once the device is substantially de-risked. This typically means there is a working prototype, a clear market opportunity, and the foundational evidence that the device can perform its intended function.
Design your regulatory strategy like you design your product
It’s critical to integrate regulatory strategy and design controls early in the development process, rather than retroactively documenting decisions after the product is built. This proactive approach ensures all necessary evidence is generated in real-time and aligns product development with regulatory expectations.
At Cortex, we start with the end in mind. We bring in regulatory specialists early and integrate design controls and user validation throughout. This doesn’t just create better documentation, it creates better products.
Be thorough in the predicate research for equivalency
You may find what you think is the right predicate device, but beware that there are devices that are poorly documented, too old, or simply not doing well in the current market. Do your due diligence in your research; reverse engineer, look in the MAUDE database for recalls or complaints, and look for newer devices that are more likely to pass today’s regulations.
If you’re unsure whether a predicate is appropriate, consider submitting a Pre‑Submission (Pre‑Sub) through the FDA’s Q‑Sub program to get early regulatory feedback and reduce risk.
Be strategic with labelling and communication
Labelling extends well beyond packaging; it includes website messaging, Instruction For Use (IFU), and device markings, all of which shape how users and buyers understand and emotionally connect with your product. While not strictly required by regulators, compelling, well-planned labelling is critical for market success and also strengthens your design history file and final documentation.
Provide a high-quality submission right from the start
The quality of your first submission will dictate the likelihood of it being accepted. You want to get it right the first time; ensure that all of the components are well reviewed. This can be done by your design firm, like Cortex Design, or in conjunction with a regulatory specialist, be it one you choose or one that we provide.
Focus on market success, not just regulatory success
A cleared device doesn’t automatically translate into commercial success. Regulatory success and market adoption are two separate challenges. That’s why we pay close attention to the quality of decisions documented in the DHF, from how choices are made and validated, to how intuitive the device is to use.
“The most expensive device you’ll ever design is the one nobody buys.”
“Not all ventures are successful, but it’s our job to increase that rate of success. And that’s why we put our money where our mouth is, and sometimes we invest in the ventures that we’re involved in. We want to be part of that success, and we are motivated to be your partner with that.”
To Consider: The Changing FDA Environment
With shifts in FDA leadership and tightening budgets, reviewers today often carry heavier workloads with fewer resources. There’s a lot of talk about implementing AI tools to aid in their process, and this could be a good or bad thing. Regardless of what this means, your submission needs to be crystal clear, well-organized, and easy for them to process. Making it easy for FDA reviewers to do their job is one of the smartest ways to ensure a smooth review.
510(k) FAQs
When should you start thinking about the 510(k)?
How do you file?
What if there’s no predicate?
How much does a 510(k) cost?
What’s the difference between a 510(k) and a De Novo?
How long does it take to get 510(k) clearance?
Once submitted, the FDA’s goal is to make a decision on a 510(k) within 90 FDA days—which excludes any time the submission is placed on hold due to questions, requests for additional information, or required revisions. In reality, the review timeline often stretches beyond that.
That’s just the regulatory review. Getting to submission is another story.
The device development journey—from functional prototype to a complete 510(k) submission—typically takes 12 to 36 months, depending on complexity. At Cortex, we usually complete this process in 9 to 18 months.